




Our smiles are built to last. In fact, tooth enamel — the outer surface of our teeth — is the hardest substance in the human body, stronger even than our bones. That tooth enamel can withstand a lot of wear and tear. But as we live longer, and expose our teeth to stresses like clenching, grinding or chewing on hard objects, we can put our smiles at risk. If you think you have a cracked tooth, it's important to seek treatment quickly, before the problem gets worse.
- How do I know if my tooth is cracked?
- Why does a cracked tooth hurt?
- What if my tooth is chipped?
- How will my cracked tooth be treated?
- Will the tooth heal completely after the treatment?
- What can I do to prevent my teeth from cracking?
How do I know if my tooth is cracked?
Cracked teeth show a variety of symptoms, including erratic pain when chewing, possibly with release of biting pressure, or pain when your tooth is exposed to temperature extremes. In many cases, the pain may come and go, and your dentist may have difficulty locating which tooth is causing the discomfort. Αρχή άρθρουWhy does a cracked tooth hurt?
To understand why a cracked tooth hurts, it helps to know something about the anatomy of the tooth. Inside the tooth, under the white enamel and a hard layer called the dentin, is the inner soft tissue called the pulp. The pulp contains the tooth's nerves and blood vessels. When the outer hard tissues of the tooth are cracked, chewing can cause movement of the pieces, and the pulp can become irritated. Eventually, the pulp will become damaged to the point that it can no longer heal itself. The tooth will not only hurt when chewing but may also become sensitive to temperature extremes. In time, a cracked tooth may begin to hurt all by itself. Extensive cracks can lead to infection of the pulp tissue, which can spread to the bone and gum surrounding the tooth.
What if my tooth is chipped?
Chipped teeth account for the majority of dental injuries. Most chipped teeth can be repaired either by reattaching the broken piece of tooth enamel or by bonding a tooth-colored filling or crown in place. See your dentist as soon as possible after the injury to treat your chipped tooth and keep it from worsening.
How will my cracked tooth be treated?
There are many different types of cracked teeth. The treatment and outcome for your tooth depends on the type, location and extent of the crack.Craze Lines
Craze lines are tiny cracks that affect only the outer enamel. These cracks are extremely common in adult teeth. Craze lines are very shallow, cause no pain, and are of no concern beyond appearances. What do we do if a piece of a tooth breaks?
Cracks / fractures make up the majority of dental injuries. Most cases are treated either by re-sealing the broken part, in case a piece of enamel is broken, or with a white filling. It is important to visit the dentist as soon as possible to avoid worsening of the condition.
Cracked tooth
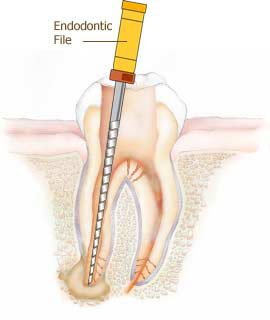
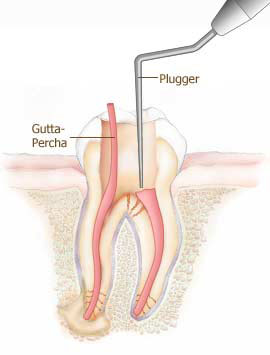
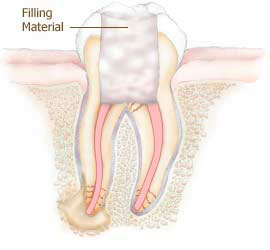
.jpg) A cracked tooth means a crack extends from the chewing surface of your tooth vertically toward the root. The tooth is not yet separated into pieces, though the crack may gradually spread. Early diagnosis is important in order to save the tooth. If the crack has extended into the pulp, the tooth can be treated with a root canal procedure and a crown to protect the crack from spreading.
A cracked tooth means a crack extends from the chewing surface of your tooth vertically toward the root. The tooth is not yet separated into pieces, though the crack may gradually spread. Early diagnosis is important in order to save the tooth. If the crack has extended into the pulp, the tooth can be treated with a root canal procedure and a crown to protect the crack from spreading.Fractured cusp
 When a piece of a tooth’s chewing surface breaks off, often around a filling, it’s called a fractured cusp. A fractured cusp rarely damages the pulp, and usually doesn’t cause much pain. Your dentist can place a new filling or crown over the damaged tooth to protect it.
If you've cracked a tooth and breathing through your mouth or drinking cold fluids is painful, bite on clean, moist gauze or cloth to help relieve symptoms until reaching your dentist’s office. Never use topical oral pain medications or ointments, or place aspirin on the affected areas to eliminate pain symptoms. Do not rinse with alcohol solutions because you might get mucosal burns.
When a piece of a tooth’s chewing surface breaks off, often around a filling, it’s called a fractured cusp. A fractured cusp rarely damages the pulp, and usually doesn’t cause much pain. Your dentist can place a new filling or crown over the damaged tooth to protect it.
If you've cracked a tooth and breathing through your mouth or drinking cold fluids is painful, bite on clean, moist gauze or cloth to help relieve symptoms until reaching your dentist’s office. Never use topical oral pain medications or ointments, or place aspirin on the affected areas to eliminate pain symptoms. Do not rinse with alcohol solutions because you might get mucosal burns.
Split Tooth
A split tooth is often the result of the long term progression of a cracked tooth. The split tooth is identified by a crack with distinct segments that can be separated. A split tooth cannot be saved intact. The position and extent of the crack, however, will determine whether any portion of the tooth can be saved. In some cases, endodontic treatment may be performed to save a portion of the tooth.Vertical crown fracture
.jpg) A vertical crown fracture is a fracture that extends from the chewing surface of the tooth to the root vertically. The tooth does not always split in two - however, the fracture may continue to expand. Early diagnosis is necessary to save the tooth. If the fracture has spread to the nerve, the tooth is treated with endodontic treatment (denervation). However, if the fracture extends below the gums, it is no longer curable, the tooth can not be saved and must be extracted. This is why early treatment is very important . A tooth that has a fracture will gradually deteriorate, resulting in tooth loss. Early diagnosis and treatment are essential for the salvation of such teeth.
A vertical crown fracture is a fracture that extends from the chewing surface of the tooth to the root vertically. The tooth does not always split in two - however, the fracture may continue to expand. Early diagnosis is necessary to save the tooth. If the fracture has spread to the nerve, the tooth is treated with endodontic treatment (denervation). However, if the fracture extends below the gums, it is no longer curable, the tooth can not be saved and must be extracted. This is why early treatment is very important . A tooth that has a fracture will gradually deteriorate, resulting in tooth loss. Early diagnosis and treatment are essential for the salvation of such teeth.Extended fracture

It is often the result of the long-term development of a fracture. It is identified by a fracture line with distinct separate sections. A tooth broken in two cannot be saved as a whole. The location and extent of the fracture determine whether a portion of the tooth can be saved. In some cases, we perform endodontic treatment to save part of the broken tooth.
Vertical root fracture

Vertical root fractures are cracks that begin in the root of the tooth and extend toward the chewing surface. They often show minimal signs and symptoms and may therefore go unnoticed for some time. Vertical root fractures are often discovered when the surrounding bone and gum become infected. Treatment may involve extraction of the tooth. However, endodontic surgery is sometimes appropriate if a tooth can be saved by removal of the fractured portion.
After treatment for a cracked tooth, will my tooth completely heal?
Unlike a broken bone, the fracture in a cracked tooth will not heal. In spite of treatment, some cracks may continue to progress and separate, resulting in loss of the tooth. Placement of a crown on a cracked tooth provides maximum protection but does not guarantee success in all cases.What can I do to prevent my teeth from cracking?
While cracked teeth are not completely preventable, you can take some steps to make your teeth less susceptible to cracks:- Don't chew on hard objects such as ice, unpopped popcorn kernels or pens.
- Don't clench or grind your teeth.
- If you clench or grind your teeth while you sleep, talk to your dentist about getting a retainer or other mouthguard to protect your teeth.
- Wear a mouthguard or protective mask when playing contact sports.
Dental abscess A tooth abscess is an acute dental inflammation that results from an infection of the teeth or the gums. It is a purulent inflammation (a pus-filled sac) characterized by the accumulation of pus in the area around a tooth root or gum. Dental abscesses can be caused by either decayed teeth or periodontitis. They are the most common cause that many patients visit dentists with severe toothache.
- Tooth abscess. The abscess (that is, the one that forms around the tip of a tooth root) is the most characteristic form of dental abscess. It occurs when the tooth pulp is infected due to caries.
- Periodontal abscess. In the case of periodontal abscess, the cause is usually severe periodontal disease (periodontitis) or gum injury. Periodontal abscess develops in the gums (gum abscess) or in the alveolar bone that surrounds the tooth.
- Tooth abscess . It is a special form of periodontal abscess that forms due to inflammation and infection of the gums around the mill of a semi-enclosed tooth. (pericoronitis).
Causes of dental abscesses
Regardless of their type, all dental abscesses are the result of a pre-existing oral infection. The formation and concentration of pus that is the main feature of an abscess is essentially a side effect of the "battle" of our body's immune system with the bacteria that have caused the infection. Pus is a mixture of white blood cells and germs (living and dead), cell fluids, and liquefied dead tissue. An abscess at the root is usually caused by severe tooth decay or injury. When decay reaches the inside or pulp of a tooth, which contains the nerves and blood supply, the pulp dies. The infection in the pulp can spread from the tip of the root to the surrounding bone and destroy bone in your jaw. An abscess between a tooth and gum usually forms when bacteria and food get trapped in an area that is hard to clean. The infection may have been caused by:- Dental caries. A tooth abscess usually develops when caries on a tooth is not treated in time before it reaches and infects the dental pulp. The bacterial infection causes inflammation and eventually death of the pulp tissues, and continues to spread through the root canals to the root (s) of the tooth. Eventually, the bacteria reach the open end of the root, leave the tooth and infect the bone around the root of the tooth, gradually creating the abscess. In addition to tooth decay, infection of the pulp and dental abscess can result from a crack in the tooth or a defective filling or crown that creates a gateway for germs to enter the tooth.
- Periodontitis. Periodontitis is a serious condition of the gums that leads to dentition and detachment from the teeth creating deep pockets between the teeth and gums. The presence of these periodontal pockets allows bacteria to enter deep between the teeth and the surrounding gums and bone, infecting them. If the infection is not treated with deep brushing of the teeth, a periodontal abscess will quickly form.
Symptoms of dental abscess
A tooth abscess is usually quite painful, and appears as a swollen area that is warm to the touch. The main symptoms associated with a dental abscess are:- Intense, persistent, and continuous toothache.
- Edema
- Pain when chewing
- Sensitivity of the teeth to thermal changes or pressure
- Visible lump on the gums near a tooth
- Outflow of pus in the mouth
- Bad taste in the mouth and bad breath
- Redness and swelling of the gums, on the jaw or face
- Difficulty of fully opening the mouth or swallowing
- Swelling of the lymph nodes in the neck
How are dental abscesses treated
Abscess drainage:
Pain relief
- Put a cold patch on the cheek. It will relieve pain and reduce inflammation of the face.
- Take a painkiller for temporary pain relief.
- Wash with lukewarm salt water. Helps drain pus, cleanses the mouth and relieves pain.
Abscess at the root of a tooth: Root canal therapy - Endodontic Treatment
Abscess between the gum and a tooth
Antibiotics
Tooth extraction
Complications that can be caused by a tooth abscess
- Tooth loss
- Spread of the infection to the soft tissues of the face (facial cellulitis)
- Spread of the infection to the bone of the lower or upper jaw (osteomyelitis)
- Spread of the infection from the roots of the upper molars to the cavities of the sinuses (sinusitis).
- Spread of the infection to other areas of the body causing sinus thrombosis, endocarditis, pneumonia, or other disorders.
- Dental abscesses that extend to the base of the mouth or throat can become life-threatening (Ludwig's angina), blocking the airway and making it difficult to breathe.















 Services
Services